The pathophysiology of cancer-related fatigue: current controversies
C. M. O’Higgins, B. Brady, B. O’Connor, Declan Walsh & R. B. Reilly. Supportive Care in Cancer 2018
Click to read the abstract
The pathophysiology of cancer-related fatigue: current controversies
M. O’Higgins, B. Brady, B. O’Connor, Declan Walsh & R. B. Reilly. Supportive Care in Cancer 2018
Fatigue is one of the most common and debilitating cancer symptoms, and is associated with impaired quality of life. The exact pathophysiology of cancer-related fatigue (CRF) is poorly understood, but in any individual, it is likely multifactorial and involves inter-related cytokine, muscular, neuro transmitter, and neuro endocrine changes. Underlying CRF mechanisms proposed include central and peripheral hypotheses. Central mechanisms include hypotheses about cytokine dysregulation, hypothalamic pituitary-adrenal-axis disruption, circadian rhythm disruption, serotonin, and vagal afferent nerve function while peripheral mechanisms include hypotheses about adenosine triphosphate and muscle contractile properties. Currently, these hypotheses are largely based on evidence from other conditions in which fatigue is characteristic. The purpose of this article is to provide a narrative review of the literature and present the current controversies in the pathophysiology of CRF, particularly in relation to central and peripheral hypotheses for CRF. An understanding of pathophysiology may facilitate direct and simple therapeutic interventions for those with cancer.
Main findings
- The definition of cancer related fatigue (CRF) which has been adopted by the American Society of Clinical Oncology Clinical Practice Guidelines is a distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer and/or cancer treatment that is not proportional to recent activity, and significantly interferes with usual functioning.
- There is no universal definition. There is no gold standard for diagnosis and quantification of CRF.
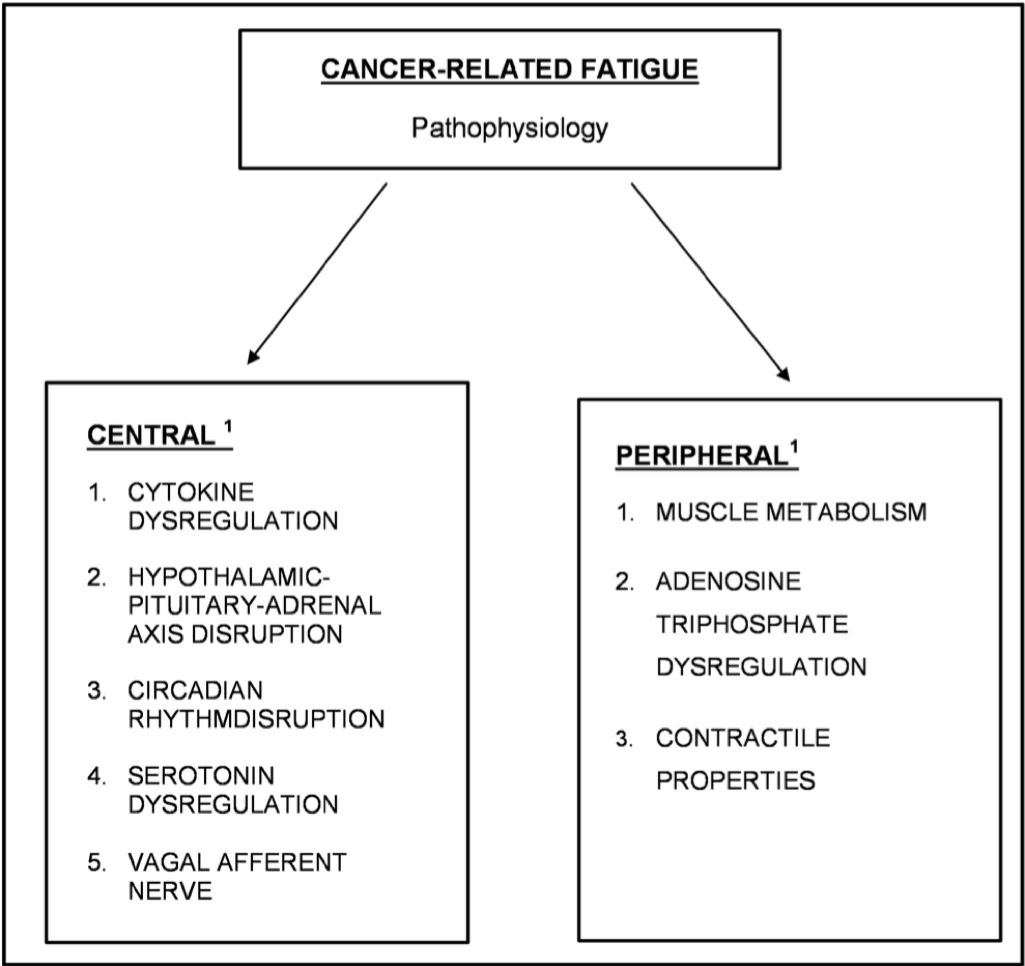
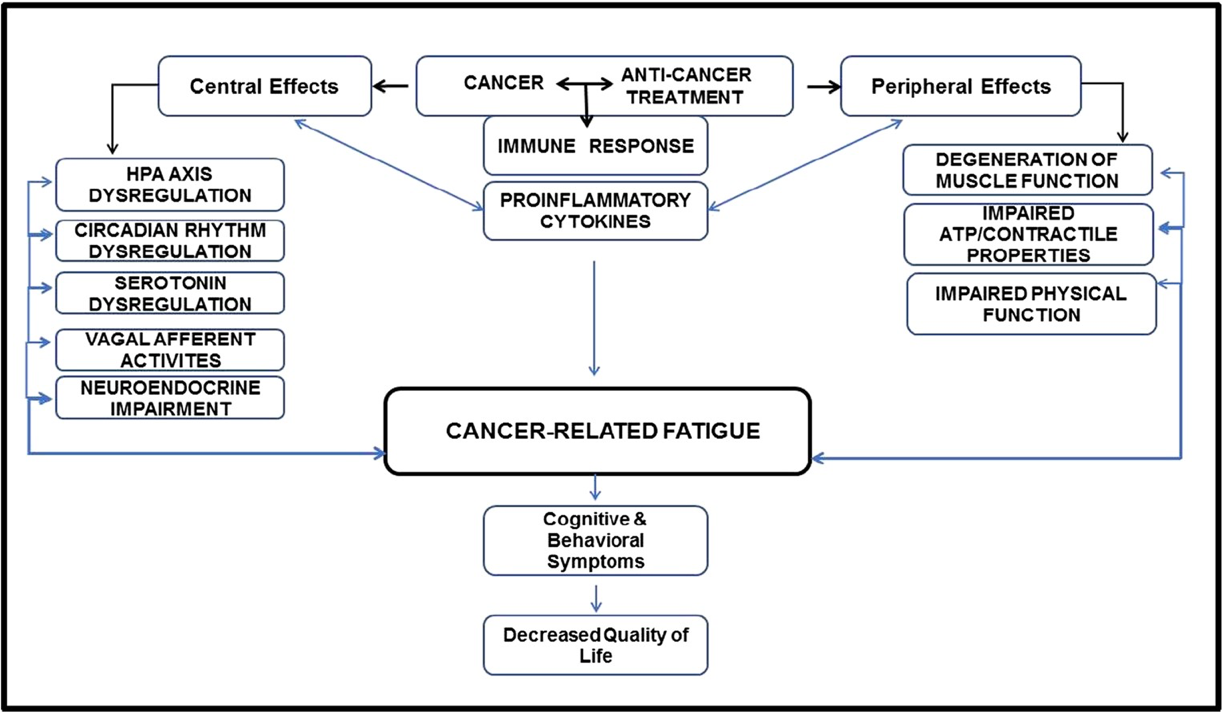
Fig. 1 Summary of proposed pathophysiology of CRF
- Cytokine dysregulation hypothesis. There is increased evidence that ongoing inflammation plays a crucial role in CRF. Cytokines are one category of signalling molecules that mediate and regulate immunity, inflammation, and hematopoiesis.
- Increased cytokine activity may occur from tissue damage after chemotherapy, radiation, or both. It is still unclear whether this cytokine activity produces or just exacerbates CRF.
- Hypothalamic-pituitary-adrenal axis disruption hypothesis. This hypothesis proposes that cancer (or its treatment) disrupts the normal HPA axis either directly or indirectly causing endocrine changes that induce CRF.
- The HPA axis has a key role in regulation of cytokine production and potent anti-inflammatory effects via a negative feedback control loop.
” Elevated cytokine levels, HPA axis, and circadian disruption can lead to CRF. - Certain cancer treatments like glucocorticoids, radiotherapy, and some chemotherapy drugs can also suppress the HPA axis, and the consequent blunted stress response may secondarily reduce energy levels.
- Circadian rhythm dysregulation hypothesis. Altered diurnal cortisol secretion and disrupted circadian rhythms are both indicative of HPA axis dysfunction, which in turn has been linked to increased cytokine signalling and fatigue in various clinical conditions.
- The current evidence therefore suggests that circadian rhythm disruption accompanied by abnormal cortisol levels are reflected in altered rest activity patterns and contribute to CRF. However, the higher cortisol levels in CRF may be secondary to stress or disrupted rest/activity cycles as a result of fatigue. Alternatively, the higher-cortisol pattern and fatigue may not be directly linked but instead triggered by a primary HPA axis disruption as cortisol is closely linked to energy production and regulation, along with many other vital behaviors and bodily functions.
- Serotonin dysregulation hypothesis. High brain serotonin (5-HT) levels or upregulation of serotonin receptors may be involved in CRF.
- Figure 3 below summarises the changes that are occurring with CRF.
Fig. 3 This review shows that cancer and/or its treatment induce a cascade of simultaneous complex biochemical, physiological, and psychological dysregulation of important biological systems in an individual. This cascade of events, in both the central and peripheral nervous system, results in cancer-related fatigue which is manifested with cognitive and behavioral symptoms, and a decreased quality of life.