
Test–Retest Reliability of Volume and Local Tissue Water Measurements in Lower Limbs of Healthy Women and Men
Charlotta Jo¨nsson, RPT, MSc,1,2 Maria Bjurberg, MD, PhD,2,3 Christina Broga˚rdh, RPT, PhD,1 and Karin Johansson, RPT, PhD1. Lymphatic Research And Biology. 2019
Abstract
Test–Retest Reliability of Volume and Local Tissue Water Measurements in Lower Limbs of Healthy Women and Men
Charlotta Jönsson, RPT, MSc,1,2 Maria Bjurberg, MD, PhD,2,3 Christina Brogårdh, RPT, PhD,1 and Karin Johansson, RPT, PhD1. Lymphatic Research And Biology. 2019
Background: Measurements of lower limb (LL) volume and local tissue water by tissue dielectric constant (TDC) are common in lymphedema management. Knowledge of normal variability in health subjects is important and can serve as a base for early lymphedema diagnosis but is currently lacking. The aim of this study was to evaluate test–retest reliability of LL volume and TDC values in healthy women and men.
Methods and Results: Thirty-three women and 28 men were measured twice, 2 weeks apart. Volume was calculated from circumferential measurements every 4cm and TDC in 14 points. Test–retest reliability was evaluated using intraclass correlation coefficient (ICC), changes in the mean, standard error of measurement in percentage (SEM%), and smallest real difference in percentage (SRD%). For volume, reliability was high (ICC 0.99) and measurement errors were low in both women and men (SEM%: 1.1%–1.3%; SRD%: 3.1%–3.6%). For TDC, reliability was fair to excellent in women (ICC 0.63–0.93) and poor to excellent in men (ICC 0.21– 0.89). Measurement errors were acceptable in all points in women (SEM%: 3.9%–10.2%; SRD% 10.8%– 28.2%), but only in 11 points in men (SEM%: 3.9%–14.5%; SRD%: 10.9%–40.1%). The points close to bone and tendons in men had lower reliability and higher measurement errors.
Conclusion: Measurements of LL volume and TDC are reliable in healthy women and men; both methods can be recommended. However, TDC points close to bone and tendons in men should be used with caution.
Main findings
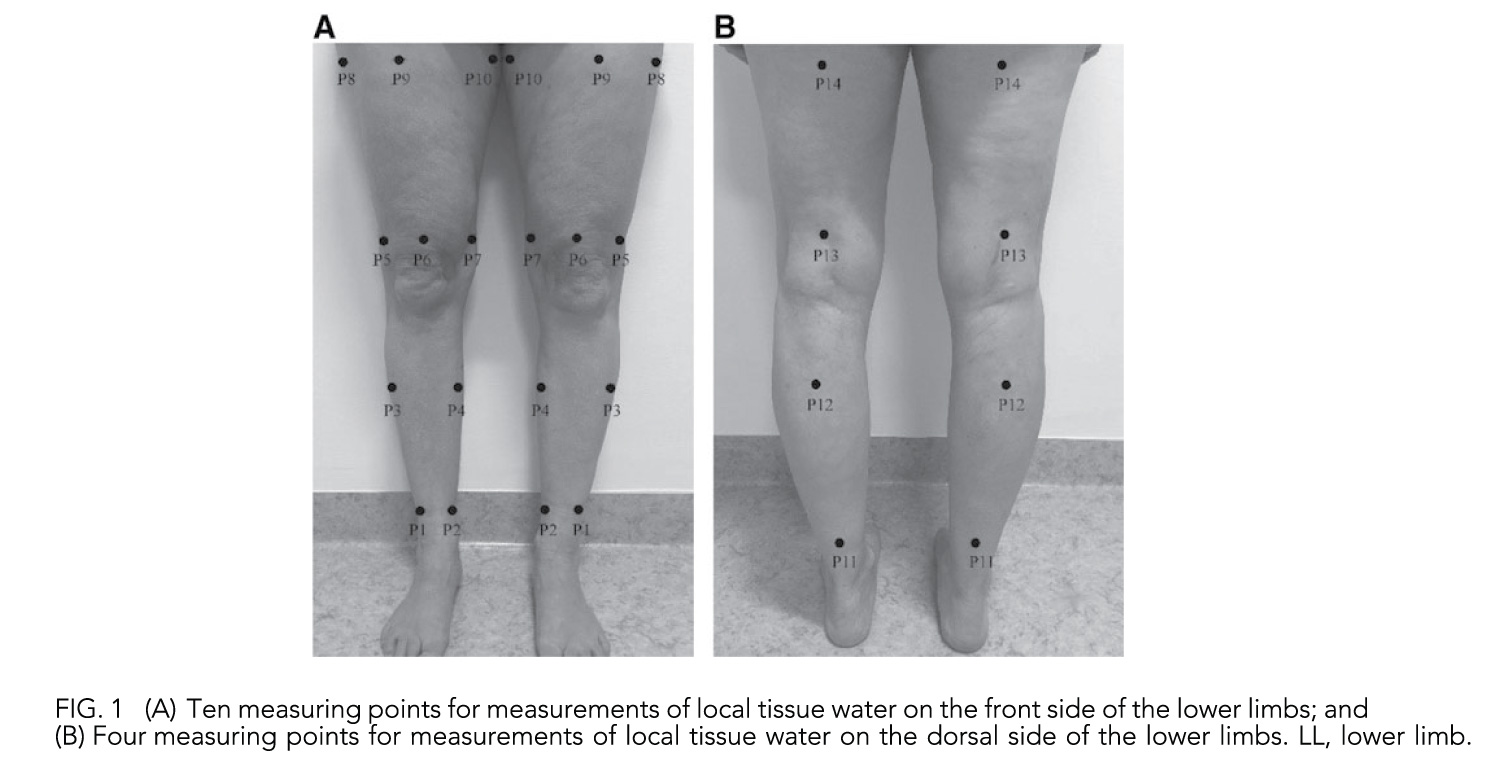
- Measuring sites for the TDC. To cover the limb a total of 14 measuring points, equally apart, were marked on each limb.
- TDC measurements the markings on the lateral, ventral, and medial side were made in the following order:
- P1/P2 was identified by placing the ruler’s short end on the measuring board at 15cm from the heel, and the most lateral/medial part of the limb was marked. To identify
- P3/P4, the distance from the heel on the measuring board was chosen for each individual to be 30, 35, or 40cm, aiming close to the widest point.
- The ruler was placed with the short end on the measuring board at the chosen distance, and the most lateral/medial part of the limb was marked. P6 was marked 3cm proximal to the base of patella.
- To identify P5/P7 the measuring tape was placed next to P6 with the tape hanging down on the lateral and medial side of the limb. P5/P7 was marked on the most lateral/medial part of the limb next to the tape.
- To identify P9, the measuring tape was placed between P6 and the anterior superior iliac spine, with the zero point at P6. The distance from P6 was chosen for each individual to be 15, 20, or 25cm and was marked. T
- o identify P8/P10 the measuring tape was placed next to P9 with the tape hanging down on the lateral and medial side of the limb. P8/P10 was marked on the most lateral/medial part of the limb.
- With the subject in a prone position, the dorsal points P11, P12, P13, and P14 were identified by placing the measuring tape between the lateral and medial points on the limb. The points were marked on the midline of both limbs. TDC measurements were taken in triplicate at each point, and the average of the two closest values was used in the analysis.
- For the circumference measurements markings were made on the lateral side of the limb with 4-cm intervals starting 10cm above the heel and ending near the groin.
- In this study the test–retest reliability of LL volume and TDC values in 14 points of healthy women and men were evaluated. We found that test–retest reliability was high (ICC 0.99) and measurement errors were low (SEM%: 1.1% to 1.3%; SRD%: 3.1%–3.6%) for LL volume in healthy women and men. For TDC, reliability was fair to excellent in women (ICC 0.63–0.93) and poor to excellent in men (ICC 0.21– 0.89). Measurement errors were acceptable in all points in women (SEM%: 3.9%–10.2%; SRD% 10.8%–28.2%), but only in 11 points in men.
- TDC points close to bone and tendons in men showed lower reliability and higher measurement errors and should therefore be used with caution.
- The analysis of the changes in the mean between the two test occasions revealed a systematic difference for TDC measurements in nine points for the L limb and in four points for the R limb in women. For the men, systematic differences in the mean were found in only two points for the L limb.
- Slightly different values for the right and the left limb. This observation also supports that each limb should be evaluated separately.
- A reliability study using the same measurement methods and the same standardized protocol in subjects with higher BMI is recommended.
- Measurements of LL volume and TDC are reliable in healthy women and men. Both methods can be recommended for a group of subjects and in single subjects. However, TDC points close to bone and tendons in men should be used with caution.

