
Reliable prediction of postmastectomy lymphedema: The Risk Assessment Tool Evaluating Lymphedema
Marten N. Basta, Liza C. Wu, Suhail K. Kanchwala, Joseph M. Serletti, Julia C. Tchou, Stephen J. Kovach, Joshua Fosnot, John P. Fischer. The American Journal of Surgery (2017) 213, 1125–1133.
Click to read the abstract
Reliable prediction of postmastectomy lymphedema: The Risk Assessment Tool Evaluating Lymphedema
Marten N. Basta, Liza C. Wu, Suhail K. Kanchwala, Joseph M. Serletti, Julia C. Tchou, Stephen J. Kovach, Joshua Fosnot, John P. Fischer. The American Journal of Surgery (2017) 213, 1125–1133.
BACKGROUND:
Breast cancer-related lymphedema remains a significant complication post mastectomy. Identifying patients at highest risk may better inform targeted healthcare resource allocation and improve outcomes. This study aims to identify lymphedema predictors after mastectomy to develop a simple, accurate risk assessment tool.
METHODS:
An institutional retrospective review identified all women with breast cancer undergoing mastectomy between January 2000 and July 2013 with postmastectomy lymphedema as the primary outcome. Stepwise multivariate Cox regression identified independent predictors of lymphedema. A simplified risk assessment tool was derived and composite risk estimated for each patient.
RESULTS:
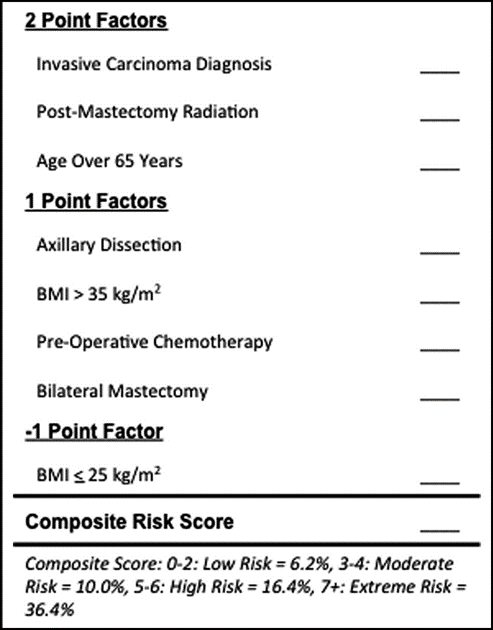
Of 3,136 patients included, 325 (10.4%) developed lymphedema after a follow-up of 4.2 years. Significant predictors included invasive cancer diagnosis (hazard ratio [HR] = 2.25), postmastectomy radiation (HR = 2.05), age over 65 years (HR = 1.90), and axillary dissection (HR = 1.79). Stratified lymphedema risk by group was defined as follows: low 6.2%, moderate 10.0%, high 16.4%, and extreme 36.4%. The model demonstrated excellent risk discrimination (C = .78).
CONCLUSIONS:
Postmastectomy lymphedema incidence was 10.4%. Invasive cancer diagnosis, chemoradiation, and axillary dissection imparted significant risk. The Risk Assessment Tool Evaluating Lymphedema offers accurate risk discrimination ranging from 6.2% to 36.4%. Selective treatment approaches may improve outcomes and delivery of cost-effective healthcare.
The risk assessment tool from this publication is shown below
Main findings
- This study is limited by the fact that it is a retrospective study and utilised ICD 9 diagnostics codes in the medical record. Inaccurate or missed diagnoses is possible.
- It is unclear from reading this paper why axillary dissection was scored less points compared with diagnosis and post mastectomy radiation. A description of post mastectomy radiation isn’t included.

