
Late Soft Tissue Complications of Head and Neck Cancer Therapy: Lymphedema and Fibrosis
Jie Deng, Elizabeth M. Wulff-Burchfield, Barbara A. Murphy. J Natl Cancer Inst Monogr (2019)
Click to read the abstract
Late Soft Tissue Complications of Head and Neck Cancer Therapy: Lymphedema and Fibrosis
Jie Deng, Elizabeth M. Wulff-Burchfield, Barbara A. Murphy. J Natl Cancer Inst Monogr (2019)
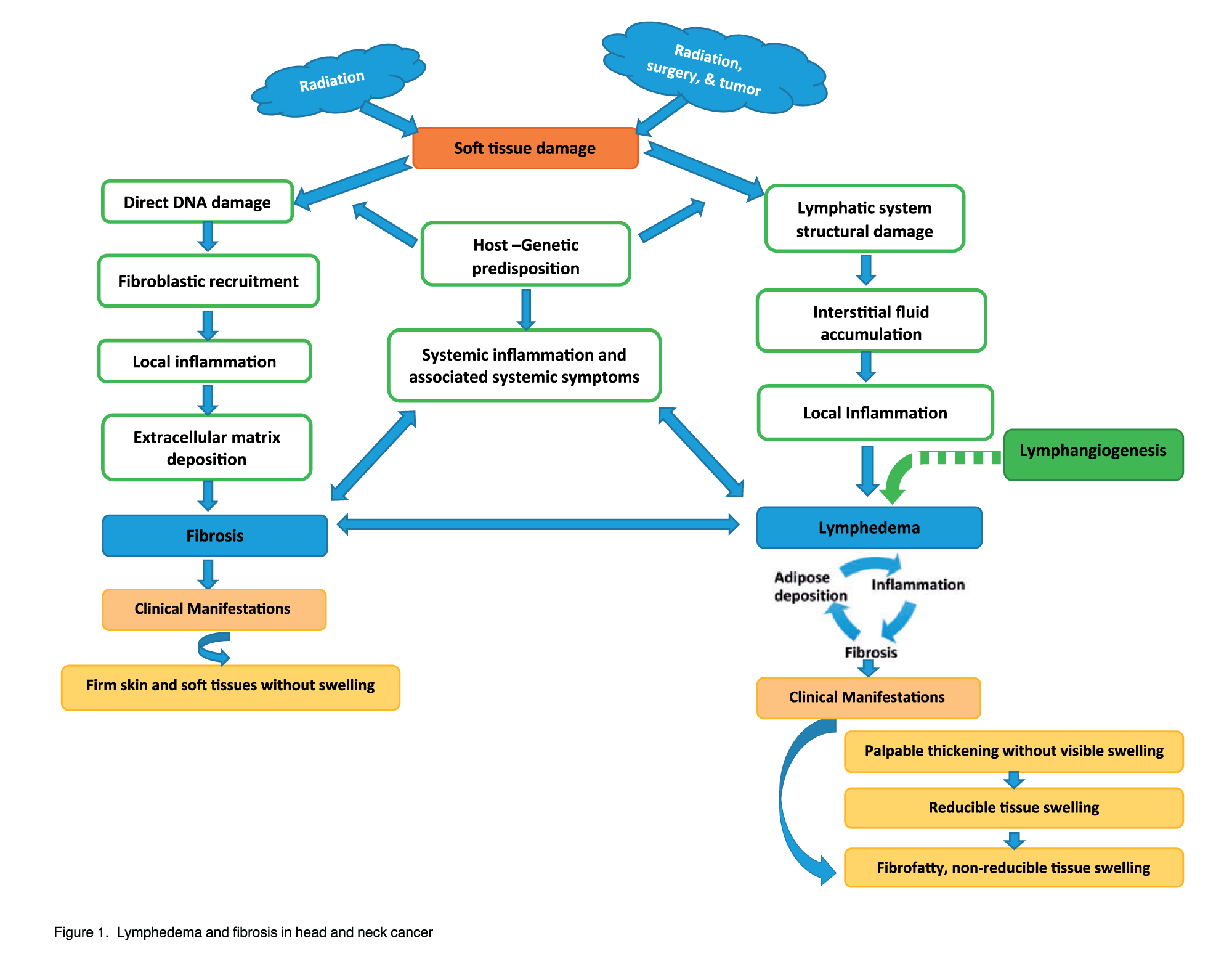
Head and neck cancer and its treatment result in soft tissue damage secondary to lymphedema and fibrosis. Lymphedema is the result of pathological accumulation of interstitial fluid in tissues. It is caused by the inability of the lymphatic system to transport lymph fluid from the tissues to the central circulatory system and is manifested clinically by tissue swelling. Fibrosis is defined as an overaccumulation of fibrotic tissues within the skin and soft tissues after a single or repetitive injury and is characterized by hardening of the soft tissues with associated loss of elasticity. Lymphedema and fibrosis are common yet overlooked late effects of head and neck cancer and its therapy. They may result in profound long-term symptom burden, loss of critical functions, and altered quality of life. The following review will discuss the current pathobiology, clinical manifestations, and future directions for research related to lymphedema and fibrosis.
Main findings
- Lymphatic fluid stasis results in a dramatic increase in the number of mixed inflammatory cells within all layers of the affected tissues. In the murine lymphedema model, a statistically significant increase in T-helper, T-regulatory, and dendritic cells, as well as neutrophils and macrophages, can be observed.
- Macrophages have an antifibrotic role in lymphedema and either directly or indirectly regulate and control CD4þcell accumulation and T-helper 2 (Th2) differentiation (17). The presence of CD4þ cells appears to be necessary for development of fibrosis and lymphatic dysfunction. Depletion of CD4þcells markedly decreases the pathological changes associated with lymphedema, including inflammation, fibrosis, and adipose deposition.
- Whereas early studies suggested that the incidence of secondary lymphedema after HNC treatment varies from 12% to 54%, a more rigorous cross-sectional report found that 75% of HNC patients after more than 3 months of posttreatment had secondary lymphedema. The high incidence of LEF has been confirmed by a recent prospective report indicating that almost 100% of HNC patients develop LEF at some point during HNC treatment and recovery.
- HNC patients frequently manifest lymphedema at one site and fibrosis at another. For example, patients frequently develop facial and submental lymphedema concurrent with neck fibrosis. Whether this reflects the propensity of specific tissue to respond to damage in a specific way, or whether it is a reflection of the density, behavior, or sensitivity of lymphatics within a select anatomical site is unknown.
- The authors have have developed a clinical assessment tool in which four types of soft tissue change were defined based on the tissue characteristic noted on physical examination: (1) dermal thickening without soft tissue swelling or fibrosis (early-stage tissue damage); (2) visible tissue swelling that is reducible, soft, and fluctuating in nature; (3) visible tissue swelling that is firm, nonreducible, and without fluctuations; and (4) hard tissue without swelling. The reporting system allows for documentation of the type and severity of abnormalities within nine defined anatomical sites in the head and neck region.
- It may be hypothesized that many late effects of therapy are due to soft tissue abnormalities caused by LEF. First, LEF causes unique sensory abnormalities that have been poorly described in the historical literature. This includes symptoms such as tightness, numbness, heaviness, and warmth (80). In addition, LEF is associated with loss of tissue compliance and plasticity resulting in statistically significant functional deficits.

