Clinical features, microbiological epidemiology and recommendations for management of cellulitis in extremity lymphedema
Jose R. Rodriguez, Frank Hsieh, Ching‐Tai Huang, Tai‐Jung Tsai, Courtney Chen, Ming‐Huei Cheng. J Surg Oncol. 2019;1-12
Abstract
Background: This high volume, single center study investigated the prevalence, bacterial epidemiology, and responsiveness to antibiotic therapy of cellulitis in extremity lymphedema. Methods: From 2003 to 2018, cellulitis events from a cohort of 420 patients with extremity lymphedema were reviewed. Demographics, lymphedema grading, symptoms, inflammatory markers, cultures and antibiotic therapy regimens were compiled from cellulitis episodes data. Univariate and multivariate analyses were performed for detailed analysis.
Results: A total of 131 separate episodes of cellulitis were recorded from 43 (81.1%) lower limb and 10 (19.9%) upper limb lymphedema patients. The prevalence and recurrence rates for cellulitis in lymphedema patients were 12.6% (53 of 420) and 56.6% (30 of 53), respectively. The most common findings were increased limb circumference (127 of 131; 96.9%) and abnormal C‐reactive protein (CRP) level (86 of 113; 76.1%). Blood cultures were obtained in 79 (60.3%) incidents, with 9 (11.4%) returning positive. Streptococcus agalactiae was the most isolated bacterium (5 of 9; 55.5%).
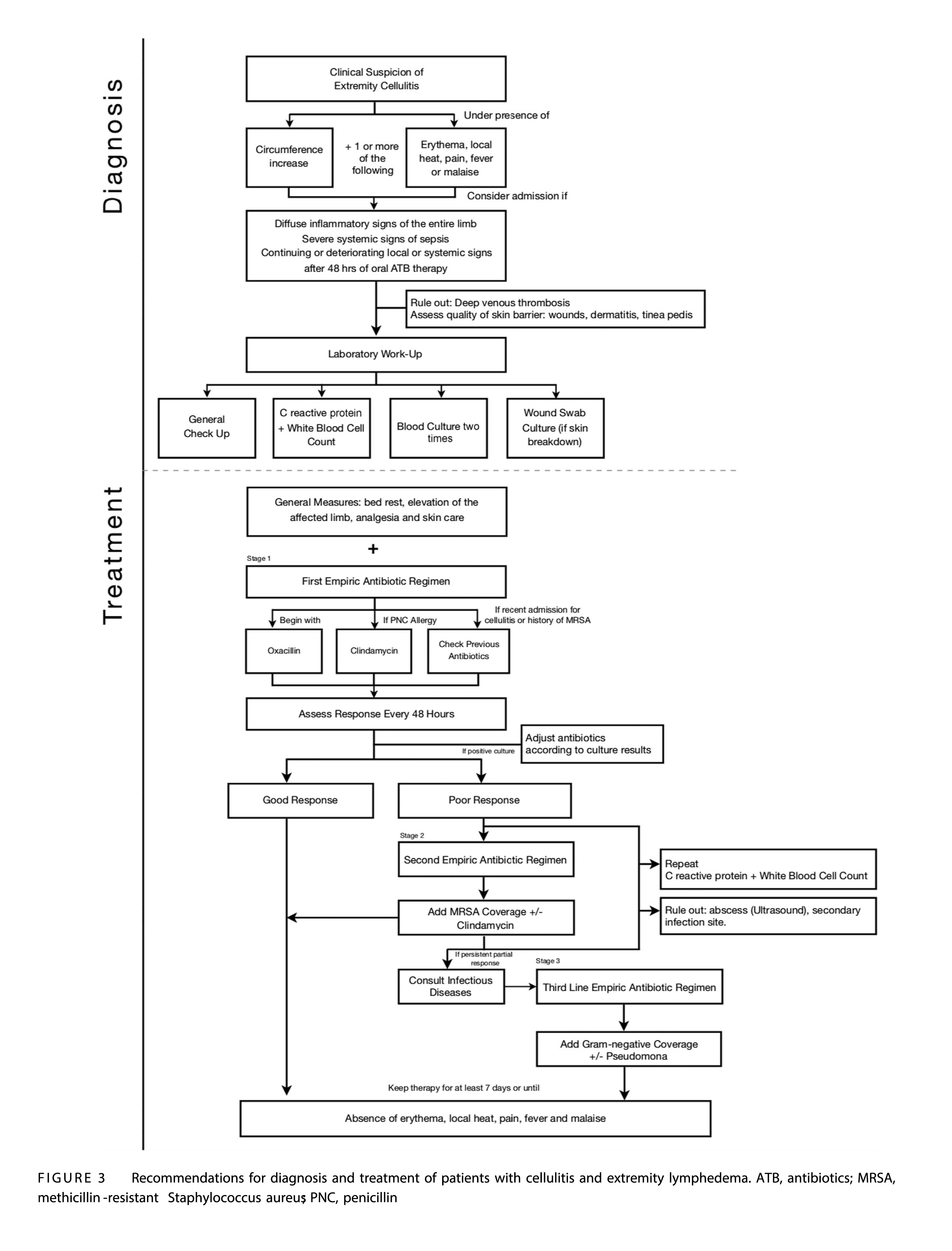
Conclusions: The cellulitis prevalence and recurrence rate in extremity lymphedema were 12.6%, and 56.6%, respectively. Strongest indicators of cellulitis were increased affected limb circumference and elevated CRP level. Empiric antibiotic therapy began with coverage for Steptococcus species before broadening to anti‐Methicillinresistant Staphylococcus aureus and anti- Gram negatives if needed for effective treatment of extremity lymphedema cellulitis.
Main findings
- Once bacteria have colonized in lymphedematous tissue, eradication is difficult, with a possibility of reactivation from latency if local immunity becomes further impaired. Some postulate that bacterial toxins accumulated in insufficiently drained lymphatic tissue may contribute to the systemic symptoms found in some patients with cellulitis and lymphedema. Cellulitis in lymphedema patients is presumed to be caused mainly by non-group A streptococci, but the pathogen is not identified in more than 80% of the cases.
- The dynamic between cellulitis and lymphedema behaves in a detrimental, self‐propagating cycle: a pre‐existing lymphatic defect predisposes to cellulitis, then episodes of cellulitis damage the lymphatic system, resulting in worsening lymphatic defects increasing susceptibility for recurrent episodes of cellulitis.
- This study found that inflammatory markers, especially CRP, were useful as adjuncts in an overall clinical picture to evaluate the degree of systemic compromise. In this series, nearly 40% of the episodes had CRP values greater than 10 times standard normal values. Reduced clearance of bacterial components may trigger the cytokine cascade, inducing a more pronounced local and systemic inflammatory response.
- It has been postulated that the aetiology of cellulitis in lymphedema patients is mainly attributed to non‐group A Streptococci strains.
- Patients with extremity lymphedema appear to exhibit a higher rate of positive blood cultures compared to the normal population.
- A summary of our current recommendations for the diagnosis and treatment of patients with cellulitis and lymphedema is presented in in the diagram below.
- This article summarizes a large single centre experience for the diagnosis and treatment of patients with cellulitis and extremity lymphedema for over a decade. The prevalence rate of cellulitis in extremity lymphedema was 12.6% with a recurrence rate of 56.6%. An increase in the circumference of the affected limb and high CRP level were the most common clinical findings. Systemic involvement was frequent. Empiric antibiotics therapy began with coverage for Streptococcus species before broadening to anti‐Methicillin‐resistant Staphylococcus aureus and anti‐Gram negatives if needed for effective treatment of extremity lymphedema cellulitis.