Obesity – The Roller Coaster
How can we assist? Or can we make it worse?
Maree O’Connor, Physiotherapist interviews the Author, Monique Lisbon and her General Practitioner, Dr. Bronwen McGraw
It is well known and researched that obesity can increase your risk of lymphoedema following lymph node removal for cancer management and aggravate established lymphoedema and lipoedema. Increasingly we are also seeing another group of clients who have leg lymphoedema due to being morbidly obese and the inguinal lymph nodes being compromised from the weight of their pendulous abdomen.
Weight management must be part of the lymphoedema/lipoedema management plan. There are roughly two types of weight management education we have with our clients. The first, for those who are not overweight, focuses on why it’s important to stay at a healthy weight range. The other is for those who are overweight and this discussion can be more complex.
For this group, there are several subgroups. There is one group who may have increased their weight because of cancer management but before this, they were always within a healthy weight range. Often these clients will be able to reduce their weight. For those who can’t and for those who have always struggled with obesity the issues are much more complex.
A common dialogue when discussing weight management with clients who are obese is the roller coaster they have had with managing their weight.
I have been to Weight Watchers and lost 50kg but have put the weight back on. I have been back several times and the same thing happens. I have also tried other programs but it always ends the same way.
The ketogenic diet was great in the short term and I lost heaps of weight but long term it hasn’t worked.
So why don’t these types of weight management programs work for many people? It is easy for us to just think that these individuals just don’t stick to the program and need to try harder. Weight management programs will never work for a lot of people because they don’t address the most important issue which is why they put the weight on in the first place. This has got nothing to do with eating.
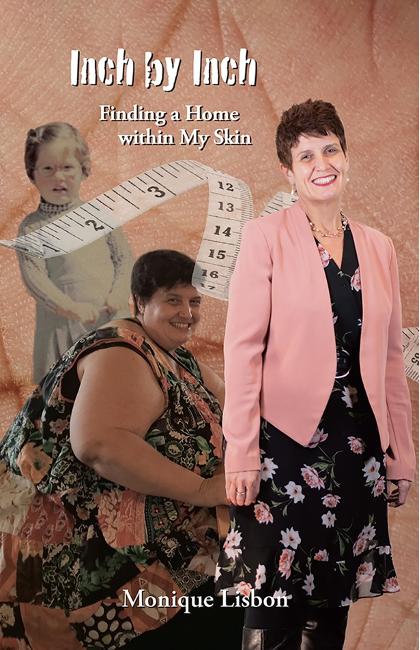
I recently read a book entitled Inch by Inch. Finding a Home within My Skin (Living Hope Resources: Ashburton, 2020).
This is written by a woman who has struggled with management for her entire life. You may be thinking “another weight management story – how will it make any difference?” It is a success story, so far, but as I was reading it I came to a better understanding of why weight reduction programs fail and how what I say and advise can have a huge impact both positively and in some cases negatively on the success of that person’s ability to lose weight. I also became worried that what I said as part of my assessment and ongoing client education could have a negative impact on that individual.
I am very fortunate that the author of this book is one of my clients and she has an amazing general practitioner (Dr. Bronwen McGraw of Zest Medical Centre, Ashburton), who has supported her through her weight management struggles. I wanted to learn from them and this is what I have found out.
Maree: Why do you think the weight management programs you have attended over the years have failed?
Monique: I think that the bulk of weight management programs don’t go deeply enough. People don’t just wake up one day and find they’re morbidly obese. The causes of obesity are usually complex and multi-faceted, and addressing the symptoms rather than the core reasons behind the obesity, can only go so far. For me, it took years to get to a point of being able to grapple with the issues behind my obesity. It then took years more to find a way through the myriad barriers to me losing weight, physically, psychologically, emotionally and relationally.
Maree: As a lymphoedema practitioner, we will discuss the fact that the individual needs to be at a healthy weight range. Often clients who are overweight say that they have tried lots of programs and they haven’t helped and they don’t each much anyway. We can suggest a dietician but for some this hasn’t worked either. Where to next?
Bronwen: It’s important to take an evidence-based approach when discussing weight loss. Diet and exercise are always important but on their own they rarely result in significant weight loss for someone who is obese. I think patients should be made aware of this and given all of the available information regarding other tools that can assist them. This may include medication, meal replacement diets and surgical options.
Maree: What do you think was the turning point for you?
Monique: There was both a negative and a positive turning point for me. The negative turning point was finding myself nearly in a wheelchair because of severe osteoarthritis in my knee that could not be addressed in any other way than losing weight. The positive turning point was the inspiration of a friend who had originally been even larger than me, but lost a massive amount of weight. Until that point, I had only read of “success stories” in books and magazines. My friend’s support, encouragement and example put a human face on the process of losing weight, and made it finally seem possible. In the end, however, if these two factors had occurred even a few years earlier, I don’t think I would have had the success I did, because I wasn’t internally ready to make the change until this point. The key turning point was finally feeling ready to make the change, and to understanding and embracing all that would involve.
Maree: In some instances, health professionals have had a negative impact on you losing weight. How has this happened?
Monique: As is the case with others in the general public, health professionals bring their own biases and prejudices. The biggest difference I felt amongst health professionals was between those who judged me, which just made me feel even more stuck, and those who felt and expressed genuine compassion towards me, which empowered me. I didn’t need to be told I had a problem – I lived with the problem every day of my life, and knew it from the inside far more deeply than anyone could observe or advise from the outside. What I needed was informed support to help me start to feel I could make a change, and steady and consistent encouragement as I made even small changes over a long period of time.
Maree: When an individual presents for the first time with a weight issue that may be impacting other medical conditions how do you start the conversation on addressing this issue?
Bronwen: This is always a sensitive topic. As Monique has already mentioned, patients are likely to be very aware of the issue but can be fearful of judgement or disappointment when they try to lose weight. I usually just try to offer hope that there are tools available now that can help, and that there is increasing evidence regarding what works for successful weight loss and weight maintenance. I always try to encourage patients that staying weight-neutral (i.e. not gaining weight) is a win (as the average weight gain is half a kilo each year) and that a small amount of weight loss has significant health benefits. For instance, losing 5% of your body weight can reduce osteoarthritis knee pain by 50%.
Maree: What tips can you provide lymphoedema practitioners in regards to discussing weight management, taking into consideration that they don’t have the skills of a psychologist?
Monique: To my mind, the key point is not assuming or implying that the answer is quick, easy, or simplistic. Even just an acknowledgment of the complexity of obesity, including the struggle to change, goes a long way. I was also helped by seeing a video that talked about understanding that I was a “victim” of my lymphoedema, not a “perpetrator”. Whilst that language may sound somewhat extreme, it did help me feel that it was not my fault that I found myself in the situation I was in. The next step, then, was to feel that I had the support and resources to make positive changes to escape the victimisation. A multi-disciplinary approach to weight management certainly helped me – addressing the issues over time with a dietician, a psychologist and an exercise physiologist – as well as with other health professionals like Maree and Bronwen. A multi-disciplinary approach helps to recognise the complexity of the issues, rather than just applying a “band-aid”.
Maree: I read in the book that at some appointments you chose not to weigh Monique. We routinely weigh our clients to check the impact of weight variation or part of doing other measurements such as bioimpedance spectroscopy via the SOZO. This may have a negative psychological impact on our clients. How do we know when this will be the case? What should we do?
Bronwen: The numbers on the scale do not tell the whole picture. And weight loss is all about playing the long game. If food is a source of emotional comfort and the patient has had a tough week then it’s important not to add to their stress and sense of failure. I think it’s important to acknowledge that some weeks are tough. It’s much better to start again the next day or week, rather than to spend another day feeling guilty or disappointed.
Also the most important health benefits occur with fairly moderate weight loss. Losing 5-10% of one’s body weight can reverse Type 2 Diabetes, control blood pressure, reduce the risk of heart attacks or strokes, improve mood and digestion, increase energy levels and reduce pain. Patients can often “miss” the bigger picture when they are purely focused on a number.
Maree: Monique, you are in a positive place at the moment. You have lost over 120kg. How do you believe you can keep this being a success story for the long term and avoid the roller coaster?
Monique: I think the key to avoiding the roller coaster, is to not become complacent with my “success”. Just as recovering drug addicts recognise that they are only “clean” one day at time, I need to remain conscious of my choices every day. This doesn’t mean I will never eat unhealthily or slip backwards – it just means that I need to remain as conscious as I can of what might be motivating the slips, and to remind myself of why I chose to embrace living health, and what a difference it has made in every area of my life – and then to choose, and re-choose, to live healthily.
Maree: Some may think that Monique’s story doesn’t relate to them as they didn’t have the same childhood trauma or they aren’t morbidly obese and don’t need to have bariatric surgery. They just need to lose 10kg or 20kg or 30kg of weight. But Monique wasn’t always 200kg – she started with being 10kg overweight, etc. How do you feel Monique’s story can help others?
Bronwen: Monique’s story is incredibly inspirational to both myself and to others, because she did overcome so many fears and barriers along the way. Her weight loss exceeded the amount experts said was possible. Prior to losing weight she was told that she would need a knee replacement and she was in constant pain – and now she has almost no pain and she exercises everyday.
I think her story demonstrates how important it is to individualise patient care and to have a team approach to treatment. And to never give up. As a patient or as a health professional it is important to believe in change and to empower patients to find their own path.
Maree: Finally, what message would you like to send to practitioners who manage lymphoedema/lipoedema?
Monique: I guess the main thing I would like to remind all health practitioners, is that every patient or client comes to them with a back-story. You may not know or understand their back-story, but you can rest assured that it is far more complex than can be summed up in a page or two of clinical notes. The back-story is also often even far more complex than the client themselves might know. So, I would like to see practitioners avoiding giving simplistic advice, learning to listen deeply over time, recognising their own limitations and biases, and extending compassion rather than judgment.