How can we help our clients stay on track with self-management?

Self management is an essential part of lymphoedema management as most treatment options require input from the client. There is no quick fix. But prior to discussing how we can keep our clients staying on track it’s useful to review terminology.
Compliance is the degree to which a patient deviates from professionally prescribed treatment (Paternalistic view)
Concordance is the agreement between professional and patient about treatment goals (shared views)
Adherence being the continuation of the agreed plan
To enhance adherence it’s essential to;
- acknowledge the experience;
- educate towards adherence;
- establish a treatment plan that is realistic and the client commits to;
- make sure there is both social and professional support as required.
There are increasing number of research papers on adherence and self-management. Below are the take home messages from some of the more recent articles.
Breast cancer survivors’ perspectives of critical lymphoedema self-care support needs. Ridner et al 2016.
This research explored the self-care support needs of 21 women and sheds some light on the experience of undertaking self-care. The main issues for these women were:
- Lack of resources for self-care including lack of tangible self-care support (social support) and lack of self-care supplies including lack of planned follow up and assessment of arm status. There was a lack of appreciation of the limitations and difficulties lymphoedema imposed on these individuals.
- Self-advocacy. The need to proactively plan to manage lymphoedema complications, the need to educate health care providers and the feeling of being marginalized by the health care system. Participants had to advocate for appropriate treatment because of lack of knowledge by health professionals.
Limitations of this study included small sample size and a limited demographic makeup.
Click here to read the abstract
Breast cancer survivors’ perspectives of critical lymphedema self-care support needs.
Authors:
Ridner Sheila, Rhoten Bethany, Radina M, Adair Melissa, Bush-Foster Sydney, Sinclair Vaughn
Source:
Supportive Care in Cancer. Jun2016, Vol. 24 Issue 6, p2743-2750. 8p.
Abstract:
To solicit breast cancer survivors’ perspectives on the variety of issues they face related to lymphedema self-care and identify support needs perceived as critical for managing their chronic medical condition.
Methods: Twenty-one breast cancer survivors with lymphedema participated in audio-recorded focus groups about barriers and facilitators of self-care. Transcripts were analysed using ATLAS.ti software by two coders. Triangulation of findings provided for refinement and category confirmation.
Results: Themes identified included lack of social support, lack of resources for self-care activities, and self-advocacy by default. Lack of social support subthemes were feeling misunderstood, minimization of needs, and feeling criticized. Lack of resources for self-care activities subthemes were lack of both tangible self-care support and self-care supplies. Self-advocacy by default subthemes were the need to proactively manage lymphedema complications, the need to educate health-care workers, and feeling marginalized by the health-care system.
Conclusions: Lack of support and the failure of others to recognize lymphedema as a chronic condition set this patient population apart from other patients with chronic diseases and decreases the amount of help needed to manage the condition.
Psychosocial factors associated with adherence for self-management behaviours in women with breast cancer – related lymphedema. Alcorso et al 2016.
This study assessed whether cognitive and affective psychosocial factors impacted on adherence to self-management for women with breast cancer related lymphoedema.
Summary of the outcomes were:
- Relatively low adherence to self-lymphatic drainage and compression garment compared with skin hygiene and avoiding injury. The reason for this may be that skin hygiene is already a routine part of the women’s life compared to wearing a compression garment/ self-manage which requires learning new skills and incorporating it into their routine.
- Time since diagnosis can influence adherence. There is less commitment to self-management over time as they may face barriers such as lack of time.
- It is critical for adherence that clients have adequate knowledge about lymphoedema and self-management. It is suggested that practitioners should assess the knowledge of their clients at the initial assessment and fill in the gaps so that they have adequate knowledge. Also provide them with resources.
Limitations of this research are that the data was obtained from self-report and there was no objective measure of lymphoedema diagnosis or severity. Also participants in this study were well educated.
Click here to read the abstract
Psychosocial factors associated with adherence for self-management behaviors in women with breast cancer-related lymphedema.
Authors:
Alcorso, Jessica; Sherman, Kerry; Koelmeyer, Louise; Mackie, Helen; Boyages, John; Sherman, Kerry A
Source:
Supportive Care in Cancer (SUPPORT CARE CANCER), Jan2016; 24(1): 139-146. (8p)
Abstract:
Purpose: Cognitive and affective psychosocial factors have been found to underlie adherence to preventive behaviours in women at risk of developing lymphedema following treatment for breast cancer. The aim of this study was to determine if these factors are associated with adherence to self-management behaviours for women diagnosed with breast cancer-related lymphedema (BCRL).
Methods: Women with BCRL were recruited through a community-based breast cancer organization and three Australian lymphedema treatment clinics. Participants completed an online questionnaire assessing demographics, medical history, adherence to self-management behaviours, psychosocial variables (personal control, treatment control, consequences, distress, and self-regulation of affect), and knowledge about lymphedema self-management.
Results: A total of 166 women participated in the study. Participants reported adhering to a mean of five out of seven behaviours, with 19.5% of participants adhering to all seven behaviours. Adherence to individual behaviours ranged from 65% (self-lymphatic drainage) to 98.2% (skin care). Greater knowledge about lymphedema was significantly correlated with higher adherence. Hierarchical multiple linear regression analysis indicated that only medical history factors (time since diagnosis and having undergone hormone replacement therapy) predicted a significant amount of the variance in adherence.
Conclusion: These findings highlight the importance of patient knowledge for optimal adherence to a self-management regimen. In addition, medical history factors may identify if a patient is at risk of nonadherence. The lack of association of adherence with other psychosocial factors considered in this study indicates that factors underlying adherence in affected women differ considerably from those factors prompting preventive behaviour adherence in the at-risk population.
Association between lymphedema self-care adherence and lymphedema outcomes among women with breast cancer- related lymphedema. Brown et al 2015.
This research was attached to the physical activity and lymphedema (PAL) trial. In this trial participants were randomised to either a progressive weight lifting intervention or no exercise. Those that did weight lifting wore a compression garment.
The major finding of this study is that levels of self-care adherence did not predict outcomes during 12 months. It is also suggested that twice- weekly weight lifting with a compression garment is sufficient to improve lymphoedema outcomes despite lack of adherence to other self-care modalities. There are also added health benefits to exercising. However this research doesn’t conclusively answer this question and needs to be examined in a randomised controlled trial.
Such a trial will provide us with much needed information on whether the self-care modalities we prescribe, which can often burden our clients, are effective (especially over time) or are we better off getting our clients to exercise which has many other health benefits.
Exploring patient perception of success and benefit in self-management of breast cancer-related arm lymphedema. Jeffs et al 2016.
Regardless of what self-care strategies you prescribe this article has very useful information on assisting our clients to independently self-care. Acceptance and adjustment to lymphoedema impacts on the ability for the person to self-manage. The analogy of the client moving from being a novice to an expert is excellent. As practitioners we can relate to this. Figure 5 below is an excellent table that explains the transition from novice to expert – adjusting to living with lymphoedema.
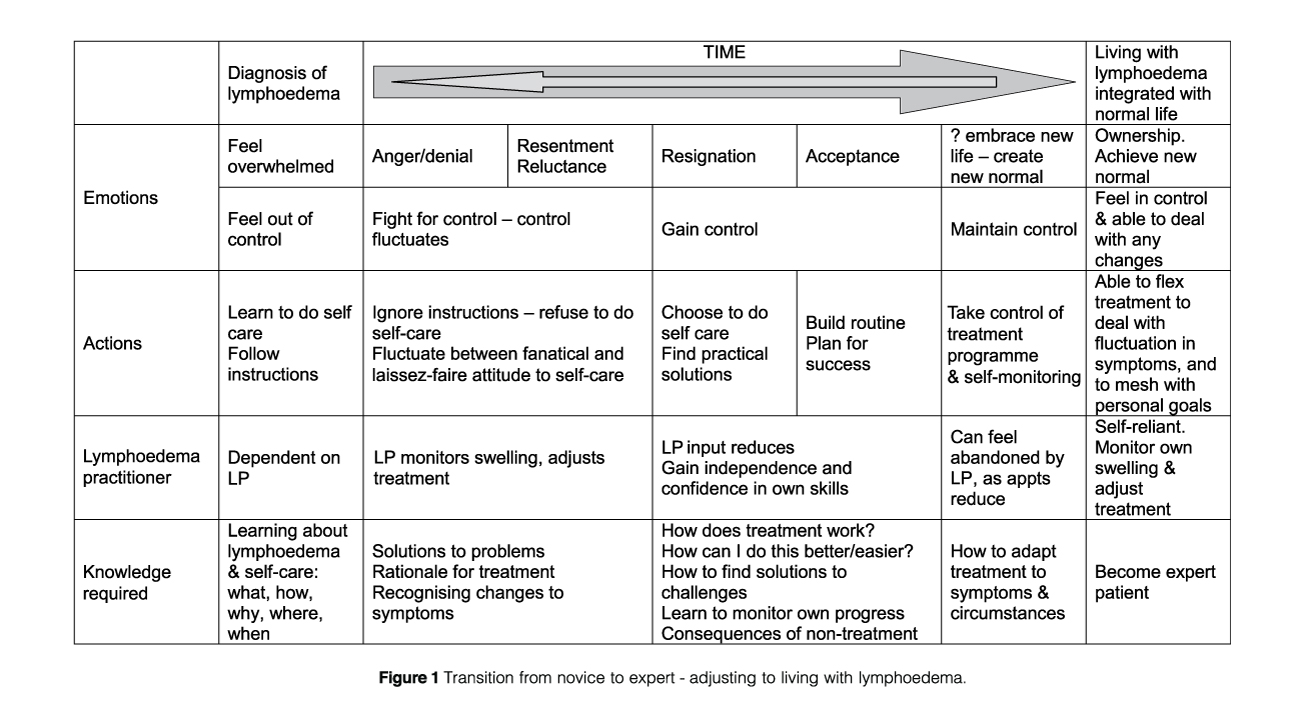
The take home messages from this article are:
- It takes time for a client to be confident and competent in managing their lymphoedema as well as be in control of their life with lymphoedema.
- Perceived treatment benefit is considered an enabler for self-management. This can be perceived differently from person to person.
- It is important to reinforce that outcomes of treatment choices may not be immediately seen. “Attitudes and beliefs about treatment have a greater impact on self-management behaviour than factors relating to the complexity or impact of treatment.”
- Sometimes our clients may not always adhere to self-management strategies if there is too much personal cost. For example removing their glove when washing up even if there is a risk of increased hand swelling.
- It is important that clients have knowledge about the mechanism of treatment and expected outcome. This will impact on perceived benefit and hence impact on adherence.
- Clients should have a good understanding on how to monitor symptoms and be confident to interpret change and how to manage this.
- Different types of knowledge are required at different stages of the lymphoedema journey (refer to Figure 1)
- Incorporating self-management activities into every day routine reduces the psychological burden of treatment. Routine assists with gaining a new sense of normal.
Conclusion
This article provides a review of the latest research. You can further expand your knowledge and skills in this area by completing lymphoedema training. Lymphoedema Education Solutions has a course that will meet your needs ranging from:
- Level 1 and Level 2 lymphoedema courses.
- Chronic oedema lower limb course.
- Lymphoedema the essentials for breast care nurses.
- Design a course to meet your needs.



